The earth’s meteorological system has witnessed extreme variations in temperature and moisture patterns across millennia, but they were not driven by a species, until now. The Intergovernmental Panel on Climate Change...


The earth’s meteorological system has witnessed extreme variations in temperature and moisture patterns across millennia, but they were not driven by a species, until now. The Intergovernmental Panel on Climate Change...
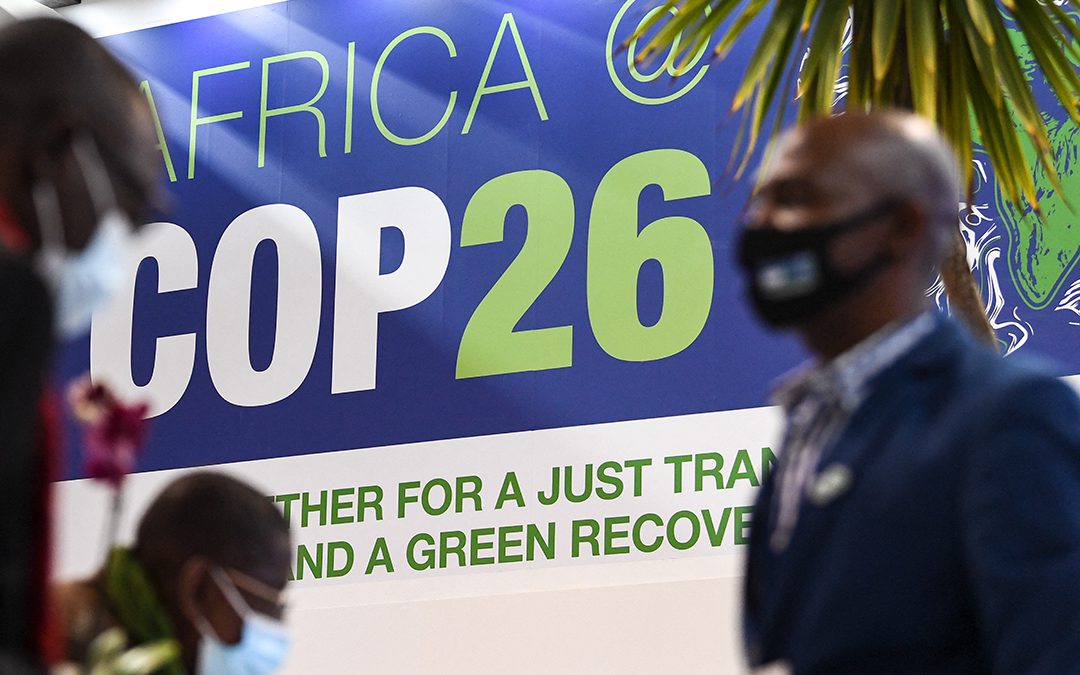
On Monday 1 November, President Uhuru Kenyatta delivered Kenya’s national statement at the World Leaders Summit of the ongoing 26th United Nations Climate Conference (COP26). As a non-permanent member of the UN...

In 2020, East Africa experienced its worst desert locust outbreak in 25 years — in 70 years for Kenya — which put nearly 40 million people at risk of food insecurity. Now, there is a new warning of desert locust hopper...

The youth make up 75% of sub-Saharan Africa’s total population. Even at a broader level, almost 200 million people aged between 15 and 24 live in Africa. It has the youngest population in the world. In addition,...

Implications for American democracy promotion and influence in Africa The 2020 US election meltdown may have dented the role and influence of America as the chief promoter and protector of democratisation in Africa....

The USA in the Horn of Africa The 9/11 terrorist attack changed the United States security strategy globally. The event took place a decade after the end of the Cold War and before the US and its allies in the West had...