During a previous African Governance Architecture meeting, the African Peer Review Mechanism chief executive Professor Eddy Maloka called for the continent to be robust and frank when dealing with governance matters....


During a previous African Governance Architecture meeting, the African Peer Review Mechanism chief executive Professor Eddy Maloka called for the continent to be robust and frank when dealing with governance matters....

Oil-rich Angola is one of the most talked-about investment destinations in Africa, but behind the economic boom there is an impoverished and disenfranchised population burdened with some of the worst social indicators...

Trust is difficult to build and easy to destroy. The same is true of democracy and good governance. Botswana has, relatively speaking, been a shining light of democracy on the continent. Until now, that is. Its recent...
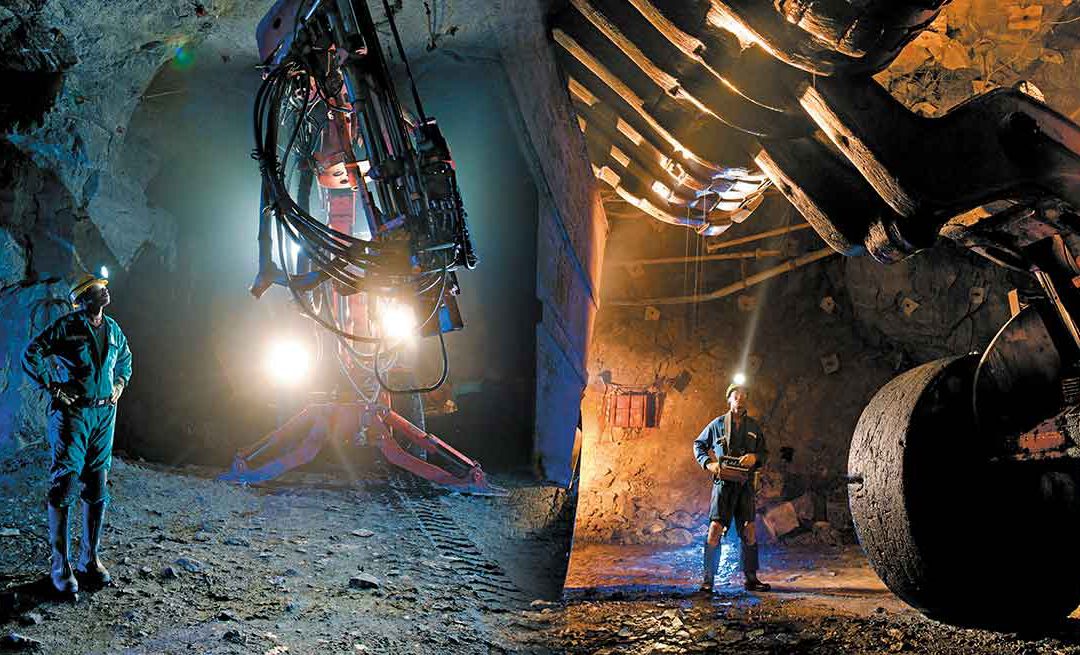
Due to the importance of critical minerals in the energy transition, the mining industry has a significant role to play in the pursuit of a net-zero future. At the same time, critical minerals mining is an...

This issue of Africa in Fact starts with a very basic premise, namely that governments cannot plan for what they do not know. Or to put it another way, “accurate, accessible and intelligible data is critical to...

Common adages in our information and knowledge-based society are that data is the “new currency” and “new oil”, powering every human endeavour. African countries have leapfrogged into the global digital economy, with...